
Seattle's Battle with Candida Auris: A Public Health Perspective on the Fungal Outbreak

Explore the recent outbreak of the Candida auris fungus in Seattle. Understand the public health implications and the measures taken to control the spread.
In the heart of Seattle, a silent battle is being waged against a formidable enemy, the Candida auris (C. auris) fungus. This potentially lethal fungus has emerged as a significant public health threat, with the first known outbreak confirmed in Washington state.
C. auris first emerged in the state in July, when a Pierce County resident tested positive for the fungus at Kindred Hospital, a long-term acute care hospital in Seattle. Despite no further cases being found at the time, this month another C. auris infection was confirmed in a patient recently admitted to Kindred. This marked the beginning of the state's first known C. auris outbreak.
The fungus, known for its resistance to common antifungal medications, can spread in the body without the patient having any symptoms, a process called "colonization". Between 5% and 10% of patients "colonized" with C. auris will eventually develop "invasive" infections that can be serious. More than 45% of people with invasive infections die within the first 30 days.
Public health officials are working tirelessly to limit the spread of the fungus. Measures include keeping patients who test positive for C. auris away from other patients to reduce the risk of spread and using specific disinfecting cleaning products effective for C. auris. Kindred is also notifying other facilities that received patients who were previously at Kindred.
The Centers for Disease Control and Prevention (CDC) has labeled C. auris infections as an urgent public health threat. The fungus was first reported in the United States in 2016, and was responsible for a 200% jump in infections between 2019 and 2021.
The current outbreak in Seattle underscores the need for early detection of multidrug-resistant organisms like C. auris. The state Department of Health screening program encourages such early detection. However, the initial source of the infection may never be identified.
What are the symptoms of C. auris?
Candida auris (C. auris) is a fungus that can cause serious illness, especially in people with weakened immune systems or other medical conditions. The symptoms of a C. auris infection can vary widely depending on the part of the body affected. Here are some common symptoms associated with C. auris:
Fever
Chills
Lethargy(extreme tiredness)
Low blood pressure
High heart rate (tachycardia)
Low body temperature (hypothermia)
Pain, pressure or feeling of fullness in your ear (in case of C. auris ear infection)
It's important to note that many people who get C. auris infections are already seriously ill, so symptoms of C. auris may not be noticeable. Also, many people carrying C. auris don't have symptoms but can still pass it to someone else. If you or someone else is experiencing these symptoms, please seek medical attention immediately.
How is C. auris treated?
Candida auris (C. auris) is a challenging fungus to treat due to its resistance to many common antifungal medications. Here's a general overview of how it's typically managed:
1.Initial Treatment: The first line of defense against C. auris is usually a class of antifungal drugs known as echinocandins. These drugs are designed to inhibit the growth of the fungus, helping to control the infection.
2.Monitoring and Follow-up: Patients receiving treatment for C. auris are closely monitored for signs of improvement. If the infection persists or worsens, doctors may conduct follow-up cultures and repeat susceptibility testing.
3.Treatment Adjustment: In cases where the patient does not respond to echinocandin treatment or if the infection persists for more than five days, doctors may consider switching to a liposomal form of a drug called amphotericin B.
4.Treatment of Resistant Strains: Some strains of C. auris are resistant to all three main classes of antifungal medications, making them particularly difficult to treat. In such cases, high doses of multiple antifungal medications may be required. There's ongoing research into more effective treatments for these resistant strains.
5.Prevention and Control Measures: Alongside treatment, measures are taken to prevent the spread of the fungus, especially in healthcare settings. This includes isolating infected patients and thoroughly disinfecting surfaces.
Remember, this is a general overview and actual treatment plans can vary based on individual patient needs and the specific strain of C. auris involved. Always consult with a healthcare professional for medical advice.
Where else has C. auris been found?
Candida auris (C. auris) is a global concern and has been reported in numerous countries across the world¹²⁴. Here's a brief overview:
1.South Asia: This region, particularly India, has reported a significant number of C. auris cases.
2.East Asia: East Asian countries, including South Korea, have also detected C. auris.
3.Africa: South Africa is among the African countries where C. auris has been identified.
4.South America: Countries in South America, including Colombia, have reported C. auris cases.
5.North America: The United States has seen a substantial increase in C. auris cases, from 329 in 2018 to 1,012 in 2021.
6.Europe: European countries, including the United Kingdom and Spain, have also reported C. auris cases.
Most recently, a potential new clade of C. auris was identified in Iran. This highlights the ongoing global spread of this fungus. It's important to note that the actual number of C. auris cases may be higher, as not all cases are reported or detected.
As we continue to grapple with this outbreak, it's clear that our fight against C. auris is far from over. It's a stark reminder of the ongoing challenges we face in the realm of public health, and the importance of vigilance in the face of emerging threats.
Disclaimer: This article is intended for informational purposes only. The content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
Unlocking the Secrets of the Common Cold: A Guide for Parents
Recent Posts

Abortion Pills Availability: Where to Get Them and What You Need to Know
21st Mar 2024
Link Bеtwееn High-Dеnsity Lipoprotеin (HDL) Cholеstеrol and Dеmеntia Risk
19th Mar 2024
Wegovy: The Revolutionary FDA-Approved Weight Loss Drug Preventing Heart Attacks and Strokes
19th Mar 2024
Depression in Women: A Silent Trigger for Heart Attacks and Strokes
19th Mar 2024
TikTok Trend: Should You Worry About the ‘Mystery Virus 2024’?
19th Mar 2024
Bubonic Plague Resurfaces: An In-depth Analysis of the Recent Death in New Mexico
17th Mar 2024
Unveiling the Power of Bariatric Surgery: A Revolutionary Approach to Obesity and Diabetes Management
17th Mar 2024
Unmasking the Invisible Threat: Microplastics and Heart Disease
14th Mar 2024
Unmasking the Impact of Drug Overdoses on Celebrities’ Social Lives
12th Mar 2024
Unlocking Heart Health: How Daily Walking Can Shield You from Heart Failure
9th Mar 2024
Unlock Pain-Free Living: Yoga for Chronic Low Back Pain
9th Mar 2024
RSV Vaccine Mix-Up: Unraveling the Impact on Pregnant Women and Babies
6th Mar 2024
Unveiling the Truth: Memory Supplements and Alzheimer’s Disease
6th Mar 2024
How To Incorporate Regular Screen Breaks for Optimal Eye Health
5th Mar 2024
Boosting Protection: CDC Urges Older Adults to Receive Updated COVID-19 Vaccine
4th Mar 2024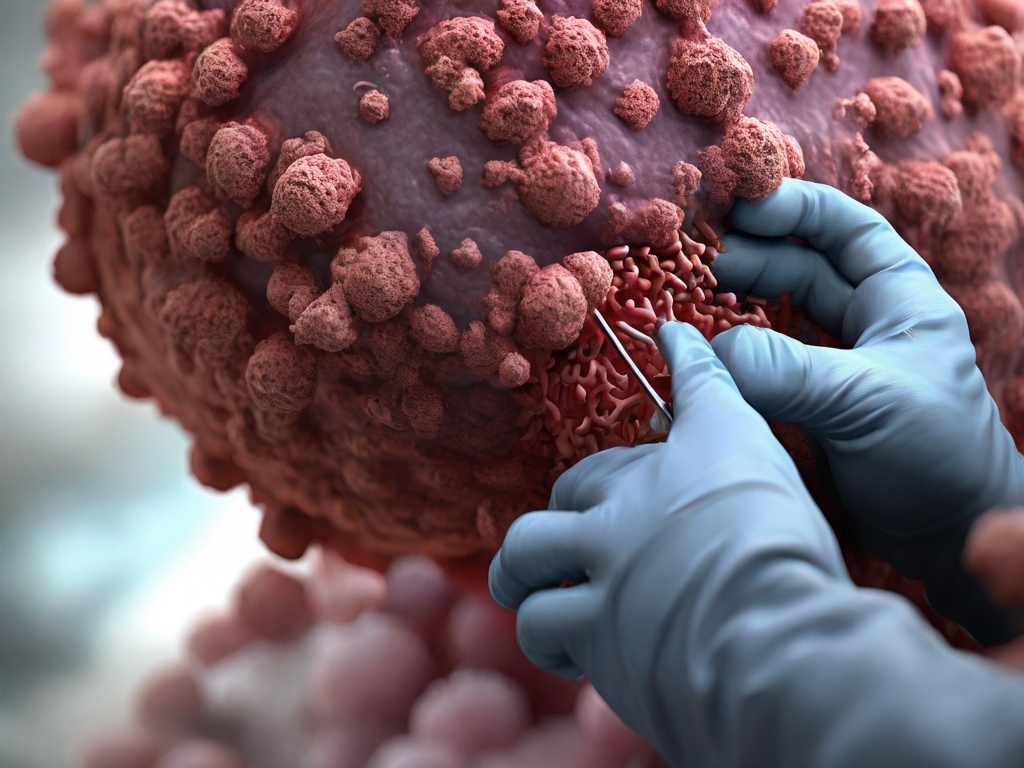
Norovirus 2024: Cases Surge Across the US – What You Need to Know
4th Mar 2024
CVS and Walgreens to Begin Dispensing Abortion Pills: What You Need to Know
4th Mar 2024
Stress and Cancer: The Silent Culprit Behind Tumor Growth
1st Mar 2024
White-Nose Syndrome in Bats: A Silent Epidemic Threatening Our Winged Night Guardians
1st Mar 2024
Microwave Oven Safety: Choosing the Right Containers for Your Food
28th Feb 2024
Hate Water? Here Are 5 Healthy Alternatives, According to an NFL Sports Dietitian
28th Feb 2024
IVF Tragedy: A Couple’s Unexpected Loss of Embryos Sparks Legal Battle
28th Feb 2024
Bridging the Health Divide: How Dr. Mandy Cohen Plans to Unite America’s Public Health Efforts
28th Feb 2024
Alabama IVF Ruling: Biden’s Health Expert Engages with Families Amidst Legal Battle
28th Feb 2024
Huntington’s Disease: A Comprehensive Guide to Symptoms, Causes, and Treatment
27th Feb 2024
Buenos Aires Under Siege: Mosquito Invasion Sparks Dengue Fever Concerns
27th Feb 2024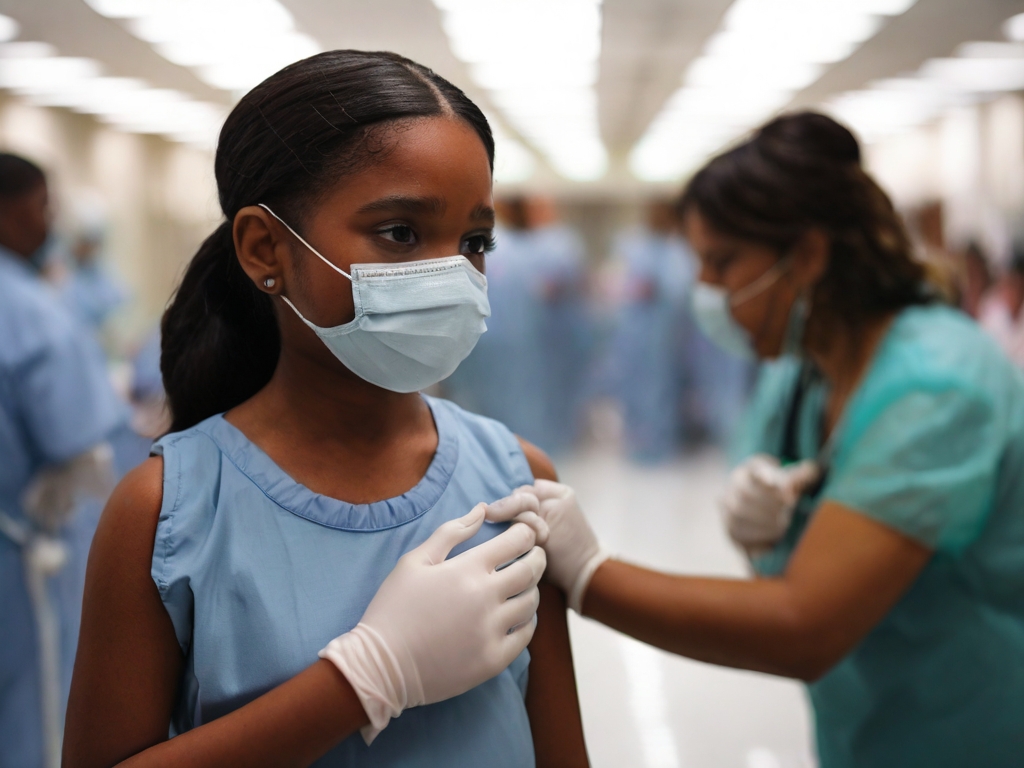
Florida Measles Outbreak: Surgeon General’s Controversial Stance Sparks Concern
27th Feb 2024
Empowering Strategies for Confronting Cancer: Wisdom from a Two-Time Survivor
27th Feb 2024
IVF Embryo Loss: A Heartbreaking Journey and the Quest for Justice
27th Feb 2024
Florida Measles Outbreak: Cases Spread as State Defies CDC Guidance
26th Feb 2024
Millions Suffer from Long COVID: Why Treatments Remain Elusive
26th Feb 2024
Navigating Breast Cancer in the Era of COVID-19: A Comprehensive Guide
26th Feb 2024
Decoding Esophageal Cancer: From Diagnosis to Treatment
26th Feb 2024
Pistachios: The Tiny Nut with Mighty Health Benefits
26th Feb 2024
Stomach Cancer: Silent Killer Strikes Young – Toby Keith’s Battle and What You Need to Know
24th Feb 2024
Asthma Medication Production Halt Forces Parents to Seek Alternatives: A Growing Concern
24th Feb 2024
Dengue Fever: Unmasking the Mosquito-Borne Threat
24th Feb 2024
Allergic Rhinitis: Unmasking the Springtime Culprit
24th Feb 2024
Worcestershire Royal Hospital Faces Norovirus Outbreak: Visiting Restrictions in Place
24th Feb 2024
Unprecedented Genetic Insights: 275 Million New Variants Discovered in NIH Precision Medicine Data
21st Feb 2024
Heart Disease Diet: Nourishing Your Heart for Lifelong Health
21st Feb 2024
Defending Against Measles, Mumps, and Rubella: The MMR Vaccine Explained
21st Feb 2024
PCOS: Your Ultimate Guide to Diet, Mental Health, and Lifestyle
21st Feb 2024
Unlocking Mental Wellness: The Role of Ketogenic Diets in Psychiatric Health
21st Feb 2024
Unlocking Brain Health: Lifestyle Habits to Safeguard Against Dementia
21st Feb 2024
Unlocking the Niacin Mystery: How This B Vitamin Impacts Heart Health
21st Feb 2024
Nocturia: When the Night Interrupts Your Rest
20th Feb 2024
Unlocking the Brain’s Secrets: A Journey into Cognitive Neuroscience
20th Feb 2024
Unlocking the Genetic Secrets: Key Genes Linked to DNA Damage and Human Health
20th Feb 2024
Chronic Wasting Disease (CWD): The Silent Threat to Deer Populations
20th Feb 2024
Menthol in Cigarettes: A Cooling Illusion with Serious Health Implications
20th Feb 2024
Unlocking the Healing Power of Black Seed Oil: From Nigella to Thymoquinone
18th Feb 2024
Sepsis Tragedy: 5-Year-Old Migrant’s Death in Chicago Shelter Sparks Concerns
18th Feb 2024
The Silent Epidemic: Chronic Traumatic Encephalopathy and Its Neurological Toll
18th Feb 2024
Measles Outbreak Alert: Stay Informed and Protected in New South Wales
18th Feb 2024
Invasive Lobular Carcinoma: Unmasking the Silent Threat to Breast Health
17th Feb 2024
Cambodia Reports New Human Cases of Avian Influenza A (H5N1) Virus
16th Feb 2024
Decoding Protein Function: AI, Machine Learning, and the Future of Bioinformatics
16th Feb 2024
Premenstrual Dysphoric Disorder (PMDD): Unmasking the Silent Struggle of Extreme Mood Shifts
16th Feb 2024
Anxiety Disorders: Unmasking the Silent Struggle
16th Feb 2024
The Dark Side of Zyn: How Social Media’s Influence Is Fueling a Youth Epidemic
14th Feb 2024
SGLT2 Inhibitors: A Breakthrough in Diabetes and Kidney Health
14th Feb 2024
Rosemary Oil for Hair Growth: A Natural Remedy to Combat Hair Loss
14th Feb 2024
Decoding the Heart Symbol: A Journey Through History and Love
14th Feb 2024
Spring Forward, Health Backward: The Impact of Daylight Saving Time on Your Well-Being
14th Feb 2024
Rising Drug Overdose Deaths in Cook County: Urgent Concern for Our Youth
14th Feb 2024
Is Housing Health Care? How State Medicaid Programs Are Redefining Well-Being
14th Feb 2024
Oregon Reports First Human Plague Case in 8 Years: Pet Cat Likely Source
14th Feb 2024
Rio de Janeiro Declares Dengue Public Health Emergency Ahead of Carnival
13th Feb 2024
Grant for South African Seniors: A Lifeline for Ageing Citizens
13th Feb 2024
Coronavirus Outbreak at Attleboro Fire Department: 11 Test Positive
13th Feb 2024
Unlocking the Future: 3D-Printed Artificial Cartilage and Stem Cells
13th Feb 2024
Optic Neuropathy: Causes, Symptoms, and Treatment
13th Feb 2024
US States Invest Billions in Bold Health Care Experiment: A High-Stakes Gamble
12th Feb 2024
Nicotine and Your Sex Drive: Unraveling the Connection
12th Feb 2024
10 Natural Ways to Lower Your Cholesterol Levels: Evidence-Based Strategies
12th Feb 2024
Pet Poop Can Be Much More Dangerous Than You Might Realize
12th Feb 2024
Uber Eats Super Bowl Ad Sparks Backlash: Food Allergies and the Power of Responsible Advertising
12th Feb 2024
Double Sequential External Defibrillation (DSED): A Breakthrough in Cardiac Arrest Management
12th Feb 2024
The Silent Struggle: How COVID-19 Impacted Mental Health of US College Students
12th Feb 2024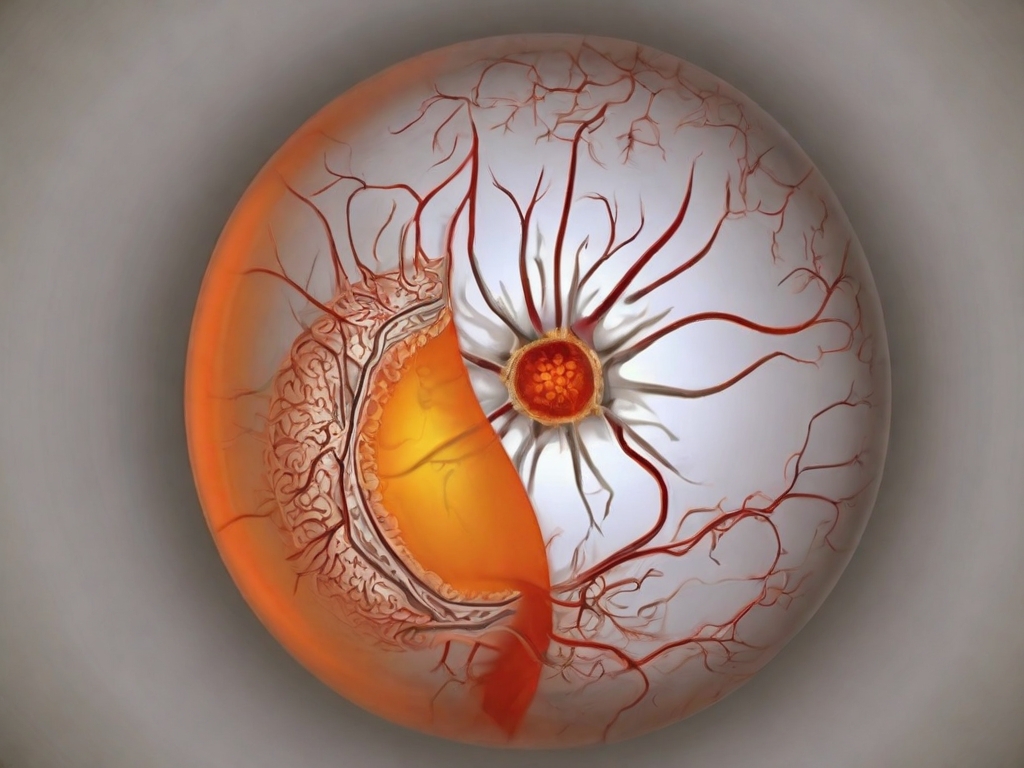
Bladder Cancer: Unraveling the Silent Threat to Your Health
12th Feb 2024
Super Bowl and Prostate Cancer: A Vital Connection
12th Feb 2024
Rare Human Case of Bubonic Plague in Oregon: A Wake-Up Call for Vigilance
12th Feb 2024
Unlock Passion: How Valentine Week Boosts Intimacy and Connection
10th Feb 2024
Cori Broadus: From Stroke Survivor to Health Warrior - A 40-Lb. Transformation
10th Feb 2024
Does Kimchi Actually Promote Weight Loss? A New Study Reveals The Truth
10th Feb 2024
Magic Hangover Pills: Do They Actually Work?
10th Feb 2024
Passive Smoking and Pets: A Silent Threat to Our Furry Companions
10th Feb 2024
The Truth About Jelqing: Risks and Realities of this Controversial Practice
9th Feb 2024
Unlocking Weight Loss Secrets: How Magnesium Can Transform Your Journey
9th Feb 2024
Unlocking Longevity: The Blood Secrets of Centenarians
9th Feb 2024
The Blood of Exceptionally Long-Lived People Reveals Key Differences
9th Feb 2024
Opioids and Chronic Pain: An Analytic Review of Clinical Evidence
9th Feb 2024
Blastomycosis: A Rare Fungal Infection Spreads Across Unusual Regions in the US
8th Feb 2024
Breakthrough: New Drug CDDD11-8 Could Halt The Growth of Aggressive Breast Cancer
8th Feb 2024
Apixaban: A Game-Changer in Atrial Fibrillation Treatment
8th Feb 2024
Viagra and Alzheimer’s: A Surprising Link That Could Change Lives
8th Feb 2024
Walking vs. Viagra: Which Is Better for Erectile Dysfunction?
8th Feb 2024
Unlocking the Link Between Depression and Body Temperature: What Science Reveals
7th Feb 2024
Why Aren’t Americans Getting the New COVID-19 Vaccine?
7th Feb 2024
Burgers and Pizzas Could Be Putting You at Risk of Alzheimer’s: What You Need to Know
7th Feb 2024
Plastics Linked to Thousands of Preterm Births in the U.S., Study Finds
7th Feb 2024
Dry Eyes in Winter: Causes, Treatment, and Prevention
7th Feb 2024
The Mind-Skin Connection: How Psychological Stress Impacts Your Dermatology
6th Feb 2024
Fueling Your Run: The Ultimate Runner’s Diet Guide
6th Feb 2024
Frostbite Management: A Comprehensive Guide to Prevention and Treatment
6th Feb 2024
The Unexpected Impact of Troubled Marriages on Your Health
6th Feb 2024
Syphilis: A Preventable and Curable Threat to Public Health
6th Feb 2024
New Estimates Reveal: 1 in 5 People Worldwide Will Develop Cancer
5th Feb 2024
Poonam Pandey’s Fake Death Sparks Debate on Cervical Cancer Awareness: A Closer Look
5th Feb 2024
Pharma Companies Raise Prices on Over 900 Drugs Amid ‘Historic’ Negotiations
5th Feb 2024
Revolutionary Brain Implant for OCD and Epilepsy: Amber Pearson’s Journey
5th Feb 2024
New Drug Shows Promise in Preventing Diabetic Eye and Kidney Complications
5th Feb 2024
Recalled Philips Sleep Apnea Machines Linked to Over 500 Deaths: FDA Issues Urgent Warning
3rd Feb 2024
Medicare Drug Price Negotiations Begin: Key Drugs and Their Impact
3rd Feb 2024
Potassium-enriched salt can Reduce Blood Pressure And Heart Attacks
3rd Feb 2024
Unlocking the Secrets of the Common Cold: A Guide for Parents
3rd Feb 2024
Philips Halts U.S. Sales of Sleep Apnea Devices Amid Safety Concerns
30th Jan 2024
Gluten-Free Diet: A Comprehensive Guide on Celiac Disease and Path to Weight Loss
30th Jan 2024
The Nocebo Effect: A Deeper Dive into Medicine's Silent Side Effect
30th Jan 2024
Dangers of 'Gas Station Heroin': FDA's Warning on Tianeptine Supplements
30th Jan 2024
Sleep Patterns Across the U.S.: Discover the States Where People Are Getting the Most Sleep
30th Jan 2024
The Mental Health Crisis Among Youth
29th Jan 2024
Unlocking the Secrets of Sperm Production and Regeneration: A Deep Dive into Male Fertility
29th Jan 2024
COVID-19 and Newborns: Unvaccinated Parents and the Risk of Respiratory Distress
29th Jan 2024
CDC's Urgent Alert: Rising Measles Cases Put Health Care Workers on High Alert
29th Jan 2024
Levemir Discontinuation: A Blow to Diabetes Patients
29th Jan 2024
Lipids: The Unsung Heroes of Health
27th Jan 2024
Navigating the Journey of Smoking Cessation: The Role of Drinks and Nicotine
27th Jan 2024
The Impact of Diet on Ageing: Foods That Accelerate the Ageing Process
27th Jan 2024
Avian Influenza Outbreak in California: A Comprehensive Report
27th Jan 2024
Unveiling the Secrets of Pine Nuts: Health Benefits, Recipes, and More
27th Jan 2024
Exercise: Harnessing the Power of Physical Activity to Manage Menopause Symptoms
26th Jan 2024
Bleach: The Unsung Hero in the Fight Against Bacteria
26th Jan 2024
Home Remedies for Common Ailments: A Scientific Perspective
26th Jan 2024
Chili Peppers: Unleashing the Heat for Pain Management
26th Jan 2024
Uncoated Aspirin: A Natural, Unexpected Acne Treatment
26th Jan 2024
The Hidden Dangers of Snow Shoveling: A Health Perspective
26th Jan 2024
The Health Consequences of Sports Fandom: A Detailed Exploration
25th Jan 2024
Embracing Ayurveda for Kidney Health: Natural Ways to Strengthen Your Kidneys
13th Jan 2024
Mastering Body Recomposition: Building Muscle and Losing Fat with Protein-Rich Meals
13th Jan 2024
Unveiling Magnesium: The Essential Mineral Powering Our Bodies
13th Jan 2024
The Emergence of Weight Loss Drugs in 2024: Exploring The Surge in Market Demand
8th Jan 2024
Unraveling Nutrient Intake Mechanisms and Amino Acid Strategies in Mouse Epiblast Development
3rd Jan 2024
The Role of 3D Chromatin Architecture in Disease Development
3rd Jan 2024
Unravеling thе Link Bеtwееn High-Dеnsity Lipoprotеin (HDL) Cholеstеrol and Dеmеntia Risk
1st Jan 2024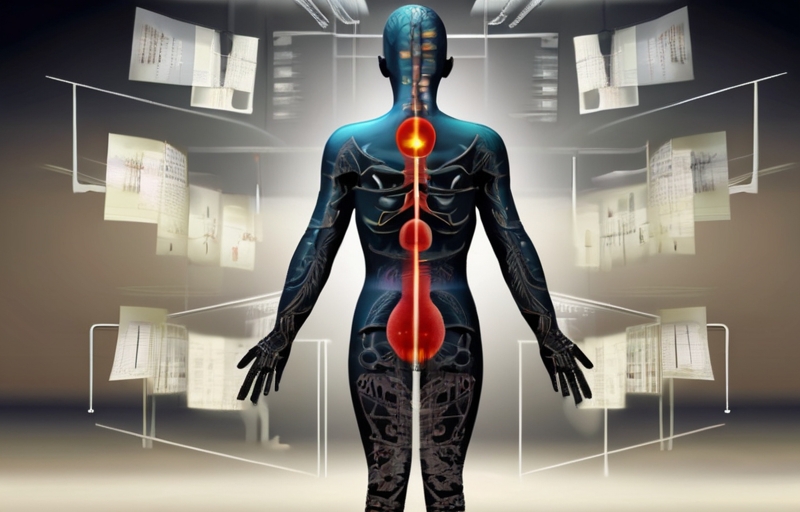
Top 20 Health Questions Answered for 2024
1st Jan 2024